Amyloid and the Kidneys
The kidneys are the most common organs involved in the systemic amyloidoses
Types of Amyloid in which the kidneys may be affected:
- AL amyloidosis
- AA amyloidosis
- Hereditary Amyloidosis mutations:
- ATTR mutation
- Apolipoprotein A1
- Afib
- AApoA
- Agel
- Dialysis related Amyloidosis. Rarely seen now with improved dialysis filtering system.
The Normal Kidney
The kidneys are extremely important organs for the daily workings of the body.
Most people have 2 bean shaped kidneys located either side of the spine below the rib cage.
Some people are born with one kidney or lose a kidney through illness or accident. The body can manage very well with one kidney.
If neither kidney is functioning death will occur quickly.
What do the kidneys do?
- Act as a filtration unit clearing waste products from the body produced during the body’s metabolism.
- Regulate body fluids and salt levels regardless of the environment a person is living in.
- Clear medications/drugs from the body.
- Regulate the body’s salt, potassium and acid content.
- Release hormones which help to control blood pressure and control calcium metabolism.
- Activate vitamin D, produced in the skin, and produce Erythropoietin (EPO) a hormone that promotes the formation of red blood cells by the bone marrow.
How do the kidneys work?
The kidneys, Ureters and bladder are part of the Urinary system.
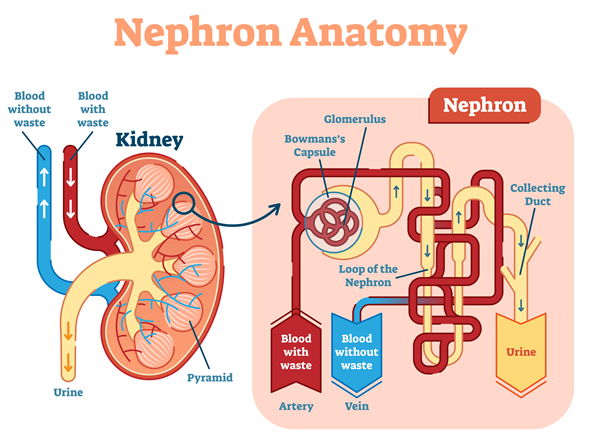
The nephron is the functional unit of filtration and collection in the kidney.
Each kidney has over a million nephrons/ filtering units.
Each nephron includes a tiny filter called a glomerulus attached to a tubule.
All the blood from the body passes through the kidneys many times each day. The kidneys filter approximately 140 quarts of blood a day.
- Blood enters the kidney through the right renal artery. This large blood vessel then branches into many smaller vessels.
- Blood flows into the nephron under pressure and enters a cluster of tiny blood vessels—the glomerulus, (the filter system).
- The thin walls of the glomerulus allow smaller molecules, wastes, and fluid—mostly water—to pass into the tubule.
- In the tubule water and chemicals are added to and removed from the filtered fluids according to the body’s needs.
- Larger molecules, such as proteins and blood cells cannot get through the barrier and stay in the blood vessel.
- The blood leaves the kidney and enters the body by the renal vein.
- The remaining waste fluid in the tubule become pre-urine which then passes through a process to become urine
- The urine then flows from the kidneys through tubes called ureters into the bladder where it is stored. When the bladder empties the urine flows out through a tube called the urethra.
- In healthy people approximately 2 liters of urine are produced every day.
More information on what your kidneys do at Kidney.org.au
Watch: How do your kidneys work? By Emma Bryce
What happens when the deposition of amyloid in the kidneys damages them?
- Renal amyloid occurs when the abnormal amyloid protein fibrils, deposit and accumulate in the kidneys over time.
The amyloid protein can be deposited in any part of the kidney but is predominately seen in the glomerulus. - Amyloid deposition and accumulation disrupts tissue architecture which then interferes with kidney function.
- The speed of progression of deposition varies depending on the type of amyloidosis.
Symptoms
Symptoms vary between patients and can be very vague.
Even when there is considerable kidney damage (up to 80%) some people experience few symptoms.
Many of the symptoms mimic other types of kidney disease and other diseases. This can result in delayed diagnosis.